More than 10% of COVID-19 patients may have symptoms which affect their quality of life or ability to perform normal activities of daily life over the long-term – upwards of 60 days. British epidemiologist Professor Tim Spector has found that 12 per cent have symptoms longer than 30 days, and one in 200 for more than 90 days. Physiotherapists have a critical role to play during recovery. “With extensive experience and research in rehabilitation, physiotherapists can help with many debilitating long-haul symptoms: breathing exercises to help the lungs recover, advice and appropriate limited exercise to keep limbs fluid and moving, counsel on managing pain and other symptoms like dizziness.” says Rogier van Bever Donker, President of the South African Society of Physiotherapists (SASP).
In practice, physiotherapists are treating patients, post COVID, for a vast array of symptoms. We now know that your symptoms may last for weeks or possibly months, especially if you have been in hospital or had severe COVID-19 symptoms. This post contains information on how to manage the following symptoms:
- Ongoing breathlessness
- Post viral cough
- Severe fatigue
- Muscle weakness
These symptoms might make it more difficult to do the things you are normally able to do, such as housework, getting dressed or walking up and down the stairs. As well as the physical symptoms listed above, it is very common to experience feelings of anxiety and low mood. Some people who have had treatment in hospital may also experience anxiety or unpleasant memories about their stay.
Managing Breathlessness
Positions to manage breathlessness
Following COVID-19 you may find you have continued breathlessness. You should monitor this and if it gets worse, seek further review from your physiotherapist or GP. These positions can help ease your breathlessness and can be used when resting or when moving around.
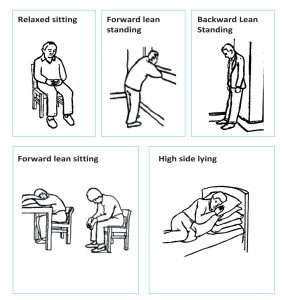
Relaxed sitting
Forward lean sitting
Forward lean standing
Backward lean standing
High side lying
Exercises to help manage your breathing
Breathing exercises can help you manage your breathlessness and reduce its impact on your everyday activities.
Breathing control:
- Take a slow breath in through your nose
- Try to relax your shoulders and neck
- Allow the air to fill up from the bottom of your lungs to the top of your chest
- Breathe gently out through pursed lips (as if you were going to blow out a candle) to create space for the next breath in
Breathing control while walking:
This will help you walk on the flat, climb stairs and negotiate slopes. Try to keep your shoulders and upper chest relaxed and use your breathing control. Time your breathing with your stepping.
- Breathe in – 1 step
- Breathe out – 1 or 2 steps
Breathe a rectangle:
Find a comfortable position. Look for a rectangle shape in the room e.g. a window, door or TV screen. Move around the sides of the rectangle with your eyes, breathing in on the short sides and out on the long sides.
Keep cool:
Make sure you have good air circulation in the room by opening a window or door. Use a wet face cloth to cool the area around your nose and mouth this can help reduced the sensation of breathlessness.
Managing your cough
A dry cough is one of the most commonly reported symptoms for COVID-19, however in some cases it may be productive of phlegm.
Strategies to manage a dry cough:
- Stay well hydrated.
- Sipping water or a soft drink – take small sips, one after the other, avoid taking large sips
- Steam inhalation – pour hot water into a bowl and put your head over the bowl. If comfortable, cover your head and the bowl with a towel.
- Drink warm honey and lemon or another warm drink, this can help to soothe the throat.
- If you do not have a drink to hand, but need to cough, try swallowing repeatedly. This can work in a similar way to sipping water.
Strategies to manage a productive cough:
- Keep well hydrated
- Steam inhalation
- Postural drainage positions as indicated by your physiotherapist. This can help to drain the phlegm
- Try moving around; this will help to move the phlegm so that you can cough it out
Exercises that can help to clear your chest
Following COVID-19 you may find that you have a productive cough and mucus on your chest. These exercises can help you to clear your chest. These may be recommended by your physiotherapist following COVID-19.
Active Cycle of Breathing Technique (ACBT) exercise consists of three breathing exercises that together help to clear the mucus off your chest.
- Breathing control
- Gentle, relaxed breathing with your shoulders relaxed
- Deep breaths
- Breath in slowly and deeply. Gently breath out without forcing it.
- Repeat 3-4 times only (too many can make you feel dizzy)
- Forced expiration techniques (Huff)
- Take a medium sized breath in
- Breath out forcefully for a short time
- Keep your mouth open and use your stomach and chest muscles
- Think ‘huffing’ a mirror to polish it

Huff coughing - Repeat 1-2 times
- Always finish on a cough or huff
- Stop when your huff is dry on two consecutive cycles
How often and how long?
- Continue to do until you feel your chest is clearer
- Clear as much mucus as you can without becoming exhausted
- Perform for at least 10 minutes, but no longer than 30 minutes
- If your cough is productive, do this 2-3 times per day
Fatigue management

You are likely to find that your energy levels fluctuate from day to day. Walking around your home might be difficult, including climbing the stairs, and managing your daily routine. This may result in you needing to adapt the activities that you do, to enable you to conserve your energy. Whilst you recover, you may need to consider a different set up, such as single level living either downstairs or upstairs. You may even require specialist equipment to make things easier. It may be useful to keep a note of how tiring different activities are for you. This will help you to understand the pattern of your fatigue and enable you to manage and adapt to this better.
Conserving your energy using the ‘four Ps’
Planning
Planning includes organising daily routines to allow completion of essential activities when you have the most energy. Many people find it more helpful to perform strenuous tasks, such as dressing, early in the day when strength and stamina are often at their peak. It is important to think about the task prior to performing the task and expending physical energy.
Consider the following:
- Think about the steps that need to be completed and items required for the task.
- Prepare the required items ahead of time.
- Keep frequently used items in easily accessible places.
- Have duplicate items available to limit unnecessary trips between the bathroom, bedroom, or kitchen.
- Consider using a bag, basket, or rolling trolley to carry tools or supplies in one trip.
- Consider your weekly routine. It will be beneficial to schedule strenuous activities, such as going to the hairdresser, attending religious services, and shopping, evenly throughout the week, instead of all in one day.
Pacing
Once activities are planned, pacing allows individuals to sustain an energy level until the task is completed.
Consider the following:
- Allow plenty of time to complete activities and incorporate frequent rests.
- Perform tasks at a moderate rate and avoid rushing. Although a task may be completed in less time, rushing utilises more energy and leaves less ‘in the bank’ for later activities.
- Allow plenty of time for rest and relaxation. Take a morning or afternoon nap prior to activities or outings to build up energy.
- Breathe easily and properly during activities. Using these techniques helps decrease shortness of breath.
- Rethink activities with rest in mind. For example, sit instead of stand while folding clothes or preparing food.
Prioritizing
The third strategy is often the most challenging. When faced with limited energy reserves individuals must look critically at work, family, and social roles and keep only those roles that are necessary and pleasurable.
Consider the following:
- Can a friend or family member assist with chores e.g. emptying the rubbish, vacuuming so you have more energy for necessary and pleasurable tasks?
- Eliminate unnecessary tasks, chores or steps of an activity. Look for shortcuts and loosen the rules.
- Being flexible in daily routines enables you to enjoy activities you would likely otherwise miss because of fatigue.
Positioning
Positioning is extremely effective, but not often considered when addressing energy conservation. Current methods of performing tasks may be using more energy than required.
Consider the following:
- Storing items at a convenient height to avoid excessive and prolonged stooping and stretching.
- Make sure all work surfaces are at the correct height. If a counter is too short, slouching and bending can occur which results in more energy expenditure.
- Use long-handled devices such as telescope cleaning tools to avoid unnecessary bending and reaching.
- Facilitate bathing – use a shower seat and a hand-held shower head.
The emotional impact
 The experience of having COVID-19 can be very frightening. It is understandable that the experience can have an emotional impact. Whether you have had mild or more severe symptoms, these are some common difficulties that you may be having:
The experience of having COVID-19 can be very frightening. It is understandable that the experience can have an emotional impact. Whether you have had mild or more severe symptoms, these are some common difficulties that you may be having:
- Feeling anxious when breathless
- Worries about health or about family or friends getting ill
- Feeling low in mood
- Poor sleep
If you were treated in hospital, you may also experience unpleasant images from your stay, nightmares or feelings of panic with any reminders of hospital.
What can help?
- Avoid watching too much news or social media if it is making you feel anxious, try limiting yourself to looking at the news once a day
- Speak to family and friends
- Try to do activities that you find enjoyable and relaxing
- Don’t be too hard on yourself if there are some things that you are finding harder to do, remind yourself that recovery takes time
- Focus on what is in your control, like eating well or doing your breathing exercises
- If you continue to feel overwhelmed by your symptoms, speak to your GP

Relaxation techniques
Relaxation is an important part of energy conservation. It can also help you to control your anxiety, improve the quality of your life and reduce pain and discomfort. Below are two relaxation techniques you can use to manage anxiety and help you relax.
Grounding technique for when you feel anxious
Take a few slow breaths and ask yourself:
- What are five things I can see?
- What are four things I can feel?
- What are three things I can hear?
- What are two things that I can smell?
- What is one thing I can taste?
Think of these answers to yourself slowly, one sense at a time spending at least 10 seconds focusing on each sense.
Picture yourself somewhere calm
Think of somewhere relaxing and peaceful. It could be a memory of somewhere you’ve been or a made up place. Close your eyes, and think about the details of this place. What does it look like:
- What colours and shapes can you see?
- Can you hear any sounds?
- Is it warm or cool?
- What does the ground feel like?
Spend some time imagining each of these.
Physical activity advice following COVID-19
Spending time in hospital or being ill at home with COVID-19 can result in a significant reduction in muscle strength, particularly in your legs. This can be for a number of reasons, but mainly due to inactivity. It’s not harmful to get out of breath when doing physical activity, this is a normal response. However if you are too breathless to speak, slow down until your breathing improves. Try not to not get so breathless that you have to stop immediately, remember to pace your activities.

You might have been given some exercises to do in hospital by a physiotherapist. Make sure to keep doing these regularly. If you are unsure about these, or you would like input from a physiotherapist, contact your local practice.


Leave a Reply